4.9. Cost of high BMI and alcohol use¶
To estimate the cost of alcohol- and obesity-related healthcare, the following steps are taken:
Estimate the per disease case cost of conditions attributable to alcohol or high BMI, including co-morbidity costs and costs of death
Estimate the obesity- and alcohol-related disease prevalence (per age, country, sex) under various policy scenarios/risk factor prevalence
Combination of the per-case cost (1) with prevalence estimates (2), to estimate the national alcohol and obesity attributable healthcare costs.
Figure Fig. 4.3 and Fig. 4.4 provide an overview of the 3-stage process outlined above for high BMI and alcohol, respectively.
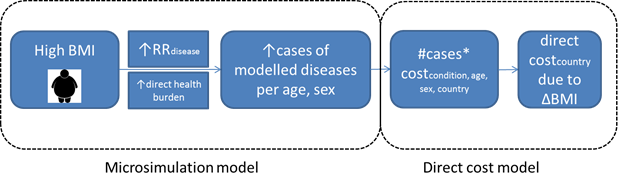
Fig. 4.3 Conceptual Framework for healthcare costs attributable to high BMI¶
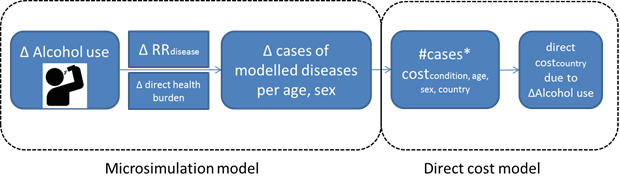
Fig. 4.4 Conceptual Framework for healthcare costs attributable to alcohol used in EU/EEA countries¶
4.9.1. Body mass index (BMI)¶
Regarding the estimation of the healthcare expenditure of obesity, in our model, BMI is associated with diseases that constitute 95% of the attributable burden via RRs (Relative Risk). For example, a person with a higher BMI has a higher risk of heart disease or low back pain compared to a person in the normal weight range. A higher BMI is also directly associated with higher morbidity. In the microsimulation model, an average higher BMI in a population results in an increased number of cases with the modelled diseases. Each case of disease is then associated with the disease specific cost, or in the case of multiple conditions, with the cost of multiple diseases, which have been estimated for all the EU/EEA countries, per age and sex. The cost of all cases in absence versus in the presence of high BMI are summed in each country, which gives the healthcare cost associated with high BMI. Alternatively, the differences in cost under various policy scenarios that alter the population BMI distribution can be modelled.
4.9.2. Alcohol¶
The healthcare expenditure model for alcohol follows a similar approach. Notably, rather than modelling a BMI range, the microsimulation model is capable of modelling alcohol use in the following ways: life abstainer/current drinker/ former drinker; alcohol consumption as continuous exposure (in g/day); and pattern of drinking (binge or not binge). To arrive at the disease burden, drinking levels are associated with disease status/mortality via RRs for alcohol related diseases, further binge drinking is also directly associated with an increased risk of disease.
It is important to note that the average age- and gender-specific costs are also estimated for individuals without any diseases. These costs are then multiplied by the number of years lived under both scenarios in order to calculate the cost difference. This cost component is necessary to account for the fact that in the absence of obesity/harmful alcohol and the associated diseases, people may still access healthcare for other, unrelated reasons.
