4.6. Cost extrapolation to other countries¶
The cost extrapolation was undertaken in three steps.
Step 1, using the information on the differentials in per capita hospitalization/outpatient/medication expenditures between the initial three anchor countries (France, Netherlands and Estonia) and the prices in the remaining EU-28 countries (where such costs were not available), the dataset containing the predicted costs for all the modelled diseases, as well as the death and residual costs in EU-28 countries was generated.
Step 2, differentials in costs between the anchor countries and all the remaining European Economic Area (EEA), plus the remaining OECD countries, plus the remaining G20 countries were estimated. This was done by regressing the disease-specific costs generated during step 1 on a number of covariates theoretically associated with the level of healthcare expenditure in each country, and then generating the predicted costs for all the countries. The cost differentials were then estimated. Note that in this step, Switzerland became a forth anchor country, as the costs were estimated for it as well.
Finally, during Step 3, costs were extrapolated from all the anchor countries to the remaining ones, but using the cost differential information estimated during step 2.
4.6.1. Step 1: Generating intermediate cost dataset for EU-28 countries¶
The aim of this step was to generate an intermediate dataset containing predicted costs for all the EU-28 countries, which could be used for regression analysis in step 2. The extrapolation was conducted from the three anchor countries where the data was initially available -France, Estonia and the Netherlands- to three EU regions: Southern Europe; Central/Eastern Europe and Northern Europe. The EU member countries were grouped into regions as follows (anchor country mentioned first):
Southern Europe (France, Croatia, Cyprus, Greece, Italy, Malta, Portugal, Slovenia and Spain
Central/Eastern Europe (Estonia, Bulgaria, Poland, Romania, Slovakia, Hungary, Latvia and Lithuania
Northern Europe (the Netherlands, Austria, Belgium, Czech Republic, Denmark, Finland, Germany, Ireland, Luxembourg, Sweden and the United Kingdom.
Our extrapolation methodology is based on the assumption that the annual treatment cost differentials between countries are time-invariant, and that they are mostly driven by the differences in two components: cost per unit of treatment received, as well as the population-level intensity of treatment provided. For example, the spending per capita for inpatient costs can be broken down as follows:
Where:
\(\frac{Spending}{Discharge}\) can be viewed as the average price per unit of inpatient treatment
\(\frac{Discharges}{Capita}\) represents the population-level ‘intensity’ of hospitalisation received in a given country.
One can divide spending per capita for inpatient treatment in a target country by spending per capita in an anchor country, and multiply the costs in an anchor country by this ratio to extrapolate to a comparator country.
Given that the cost of treatment is also determined by other components, we also estimated \(\frac{Spending}{Capita}\) ratios between countries for outpatient and pharmaceutical costs. For outpatient costs, for example, this ratio can be viewed with similar interpretation:
To estimate these differentials, we used OECD data on inpatient curative and rehabilitative care spending per capita; outpatient curative and rehabilitative care spending per capita; medical goods spending per capita. To ensure comparison and to smooth over temporary data variability, we used this data averaged over 3 years, 2012, 2013 and 2014, expressed in current prices.
To show that it’s not enough to rely on ratios of the spending per unit of care provided and that it’s also necessary to take into account the treatment intensity component, consider the case of extrapolating outpatient costs from France to Portugal.
Country |
Spending per visit, EUR |
Visits per capita |
Spending per capita, EUR |
Ratio, incorrect* |
Ratio, correct** |
|---|---|---|---|---|---|
France |
97 |
6.7 |
650 |
||
Portugal |
141 |
4.1 |
579 |
1.45 |
0.89 |
Note: Estimated as ratio of :math:`frac{Spending}{Visit}` in Portugal to France (according to :eq:`eq2_cost_extrapolation`).
The incorrect ratio of 1.45, estimated as the spending per visit ratio of costs, suggests that the outpatient costs are considerably higher in Portugal, while the correct ratio suggests that the opposite is true. The explanation is that the incorrect ratio does not take into account the population-level intensity of outpatient visits, which seem to be considerably higher in France.
After estimating the differentials in these three components, we take them all into account when estimating the overall disease-specific conversion factor between countries. It’s possible, for example, that diseases in the more acute stage, such as myocardial infarctions and strokes, have a much greater inpatient component than for example diabetes. Therefore, the overall disease-specific conversion factor to extrapolate between countries can be represented by the formula:
Where
\({x}_{i}\) is the ratio of per capita inpatient; outpatient or pharmaceutical spending between countries (based on OECD data)
\({w}_{i}\) are the weights assumed to represent treatment proportions for each disease. These weights were also obtained based on the OECD SHA data on the expenditure by disease, in millions national currency units. For example, for the Netherlands, the following table was estimated:
Inpatient |
Outpatient |
Pharma |
Inpatient, % |
Outpatient, % |
Pharma, % |
|
|---|---|---|---|---|---|---|
Ischemic stroke |
3089 |
915 |
962 |
62.20% |
18.40% |
19.40% |
Haemorrhagic stroke |
3089 |
915 |
962 |
62.20% |
18.40% |
19.40% |
MI |
3089 |
915 |
962 |
62.20% |
18.40% |
19.40% |
Cancers |
2492 |
559 |
460 |
71.00% |
15.90% |
13.10% |
Diabetes |
267 |
503 |
902 |
16.00% |
30.10% |
53.90% |
CKD |
1238 |
347 |
525 |
58.70% |
16.40% |
24.90% |
COPD |
783 |
392 |
866 |
38.40% |
19.20% |
42.40% |
Cirrhosis |
991 |
2290 |
627 |
25.40% |
58.60% |
16.00% |
Depression |
5016 |
659 |
354 |
83.20% |
10.90% |
5.90% |
Neurologic disorder |
1882 |
521 |
1475 |
48.50% |
13.40% |
38.00% |
Alcohol disorder |
1026 |
447 |
58 |
67.00% |
29.20% |
3.80% |
Remaining costs |
1 |
1 |
1 |
33.30% |
33.30% |
33.30% |
Death costs |
1 |
1 |
1 |
33.30% |
33.30% |
33.30% |
Of interest are the proportions in the last 3 columns. As one can see, for acute conditions such as strokes, MI, cancer and depression, inpatient costs indeed account for a large proportion of total healthcare costs. On the other hand, for diseases that are more chronic in nature, such as diabetes and COPD, pharmaceutical component plays a greater role. For simplicity (and due to the lack of information), we assumed that the differentials in residual and death-related costs between countries were equally driven by the differentials in the three separate components: Inpatient, Outpatient, Pharma. In addition, we assumed that in the first year of diagnosis, the differentials in more acute conditions such as strokes, MI and cancer, were driven entirely by the differentials in hospitalization costs. In the subsequent years, we assumed the weights given in Table 4.3 for all conditions.
In Table 4.3 and Table 4.4 below, examples for the extrapolation factors are shown where the costs are extrapolated from the anchoring countries (France, Estonia and the Netherlands) other countries in the same region (Italy, Bulgaria and Austria). For example, in the first year after diagnosis, the MI costs in France will be multiplied by 0.68 to predict the costs for this condition in the first year after diagnosis in Italy. In the second year, the predicting factor for this disease and this pair of countries is equal to 0.70. As mentioned in the preceding paragraph, the first year extrapolating factors for the acute conditions such as MI are different for the second (and follow-up) year ones, as we make the assumption that acute condition cost differentials are entirely driven by the hospitalisation costs in the first year.
Disease |
1st year |
2nd year+ |
|---|---|---|
Ischemic stroke |
0.68 |
0.7 |
Hemorrhagic stroke |
0.68 |
0.7 |
MI |
0.68 |
0.7 |
Cancers |
0.68 |
0.7 |
Diabetes |
0.7 |
0.7 |
CKD |
0.69 |
0.69 |
COPD |
0.69 |
0.69 |
Cirrhosis |
0.74 |
0.74 |
Depression |
0.69 |
0.69 |
Neurologic disorder |
0.69 |
0.69 |
Alcohol disorder |
0.71 |
0.71 |
Remaining costs |
0.71 |
0.71 |
Death costs |
0.71 |
Note: For example, in the first year after diagnosis, the MI costs in France will be multiplied by 0.68 to predict the costs for this condition in the first year after diagnosis in Italy. In the second year, the predicting coefficient is equal to 0.70.
Disease |
1st year |
2nd year+ |
|---|---|---|
Ischemic stroke |
0.89 |
1.12 |
Hemorrhagic stroke |
0.89 |
1.12 |
MI |
0.89 |
1.12 |
Cancers |
0.89 |
1.1 |
Diabetes |
1.25 |
1.25 |
CKD |
1.01 |
1.01 |
COPD |
1.08 |
1.08 |
Cirrhosis |
1 |
1 |
Depression |
1.1 |
1.1 |
Neurologic disorder |
1.13 |
1.13 |
Alcohol disorder |
0.89 |
0.89 |
Remaining costs |
0.98 |
0.98 |
Death costs |
0.98 |
Disease |
1st year |
2nd year+ |
|---|---|---|
Ischemic stroke |
1.63 |
1.41 |
Hemorrhagic stroke |
1.63 |
1.41 |
MI |
1.63 |
1.41 |
Cancers |
1.63 |
1.46 |
Diabetes |
1.19 |
1.19 |
CKD |
1.41 |
1.41 |
COPD |
1.32 |
1.32 |
Cirrhosis |
1.13 |
1.13 |
Depression |
1.52 |
1.52 |
Neurologic disorder |
1.38 |
1.38 |
Alcohol disorder |
1.39 |
1.39 |
Remaining costs |
1.25 |
1.25 |
Death costs |
1.25 |
While step 1 may be adequate if the goal is to extrapolate the costs from the anchor countries to the EU-27 countries only, its main disadvantage is that it does not allow extrapolation to the remaining countries (e.g. non-OECD ones, or any other countries that may be necessary to model in the future). In addition, this method suffers from two more disadvantages: the extrapolation is always done from one anchor country only, and ignores information from the remaining ones; it also relies on the assumption that overall cost differentials are only driven by the three factors mentioned above. As such, this last assumption may also lead to some induced random variation in the predicted costs, potentially driven by error rather than true differences in costs between countries. To complete the cost extrapolation exercise, we therefore implement two further steps.
4.6.2. Step 2: Estimating cost differentials between the anchor and all the remaining countries¶
Using the dataset generated during step 1, we regress country-specific costs (averaged over gender and age groups, weighted by population size in each age-gender group), on a number of covariates of interest from the World Bank dataset. Specifically, potential covariates included proportion of population aged 65 and over; log of GDP per capita; log of health expenditures per capita; GINI index of inequality; proportion of health expenditures spent out of pocket; number of physicians per capita; UHC index of access to healthcare; proportion of population living in urban areas.
To account for non-linearity of the association, as well as for the skewed distribution of the data, disease-specific GLM models with log link and gamma family were estimated. Model selection was based on automatic stepwise algorithm with a 5% threshold level chosen to keep only significant covariates. In all models, the most significant predictor was the log of health expenditures per capita. Estimated model parameters were then applied to the complete dataset (which included all the remaining countries), and the average costs were predicted for each country and disease.
Below, as an example, we show the graphical model output for one disease- alcohol use disorder. Red dots represent alcohol use disorder cost data generated during step 1, while the blue dots are those costs predicted using the GLM model. As one can see, the fit graphically looks quite good, although there is some variation in red dots around the predicted line. To smooth this variation, we rely on the differentials between the anchor country costs and all the remaining country costs using the information from the predicted, blue dot line (Fig. 4.1).
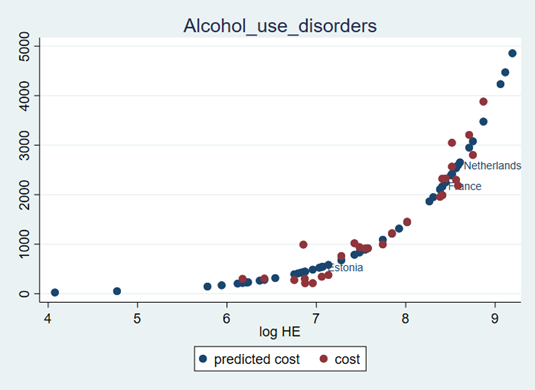
Fig. 4.1 Relationship between health expenditures per capita and alcohol use disorder costs, Euros¶
Note: The smallest predicted costs represent India and Indonesia.
Finally, disease-specific cost differentials were estimated between each anchor country and each remaining country in the complete dataset. For example, in Table 4.6 below, one can see that the average COPD costs in Austria are approximately 0.74 of that in France, 4.3 times higher in Austria than in Estonia, 1.3 times higher than in the Netherlands, and 0.66 times relative to COPD costs in Switzerland.
France |
Estonia |
Netherlands |
Switzerland |
|
|---|---|---|---|---|
Argentina |
0.243 |
1.426 |
0.415 |
0.219 |
Australia |
0.783 |
4.588 |
1.336 |
0.704 |
Austria |
0.738 |
4.325 |
1.259 |
0.664 |
Belgium |
0.705 |
4.131 |
1.203 |
0.634 |
Brazil |
0.244 |
1.428 |
0.416 |
0.219 |
Bulgaria |
0.186 |
1.092 |
0.318 |
0.168 |
Canada |
0.732 |
4.292 |
1.25 |
0.659 |
Chile |
0.279 |
1.635 |
0.476 |
0.251 |
China |
0.136 |
0.798 |
0.232 |
0.123 |
Colombia |
0.153 |
0.897 |
0.261 |
0.138 |
Costa Rica |
0.238 |
1.396 |
0.406 |
0.214 |
Croatia |
0.248 |
1.454 |
0.423 |
0.223 |
Cyprus |
0.374 |
2.194 |
0.639 |
0.337 |
Czech Republic |
0.328 |
1.921 |
0.559 |
0.295 |
Denmark |
0.838 |
4.908 |
1.429 |
0.753 |
Estonia |
0.284 |
1 |
0.484 |
0.255 |
Finland |
0.687 |
4.027 |
1.172 |
0.618 |
France |
1 |
4.034 |
1.174 |
0.619 |
Germany |
0.738 |
4.324 |
1.259 |
0.664 |
Greece |
0.361 |
2.114 |
0.616 |
0.325 |
Hungary |
0.251 |
1.469 |
0.428 |
0.225 |
Iceland |
0.677 |
3.966 |
1.155 |
0.609 |
India |
0.04 |
0.235 |
0.068 |
0.036 |
Indonesia |
0.063 |
0.37 |
0.108 |
0.057 |
Ireland |
0.761 |
4.458 |
1.298 |
0.684 |
Israel |
0.501 |
2.934 |
0.854 |
0.45 |
Italy |
0.531 |
3.113 |
0.906 |
0.478 |
Japan |
0.644 |
3.771 |
1.098 |
0.579 |
Korea, Rep. |
0.396 |
2.321 |
0.676 |
0.356 |
Latvia |
0.266 |
1.557 |
0.453 |
0.239 |
Lithuania |
0.251 |
1.472 |
0.429 |
0.226 |
Luxembourg |
0.93 |
5.449 |
1.587 |
0.837 |
Malta |
0.444 |
2.604 |
0.758 |
0.4 |
Mexico |
0.18 |
1.055 |
0.307 |
0.162 |
Netherlands |
0.772 |
4.522 |
1 |
0.694 |
New Zealand |
0.626 |
3.665 |
1.067 |
0.563 |
Norway |
1.054 |
6.178 |
1.799 |
0.948 |
Peru |
0.123 |
0.719 |
0.209 |
0.11 |
Poland |
0.232 |
1.36 |
0.396 |
0.209 |
Portugal |
0.39 |
2.284 |
0.665 |
0.351 |
Romania |
0.159 |
0.93 |
0.271 |
0.143 |
Russian Federation |
0.202 |
1.182 |
0.344 |
0.182 |
Saudi Arabia |
0.286 |
1.676 |
0.488 |
0.257 |
Slovak Republic |
0.298 |
1.747 |
0.509 |
0.268 |
Slovenia |
0.398 |
2.333 |
0.679 |
0.358 |
South Africa |
0.163 |
0.958 |
0.279 |
0.147 |
Spain |
0.475 |
2.786 |
0.811 |
0.428 |
Sweden |
0.861 |
5.043 |
1.468 |
0.774 |
Switzerland |
1.151 |
6.742 |
1.963 |
1 |
Turkey |
0.165 |
0.969 |
0.282 |
0.149 |
United Kingdom |
0.676 |
3.961 |
1.153 |
0.608 |
United States |
1.092 |
6.397 |
1.862 |
0.982 |
4.6.3. Step 3: Extrapolating to all remaining countries¶
Step 3 involves extrapolating from the four anchor countries to all the other remaining countries. For example, costs in Latvia can be predicted not only based on their differences with the costs in Estonia, but with the other countries where we have available data.
Following the logic described in generating the EU-28 dataset described in Step 1, a weights matrix
(hc_cost5 and hc_cost6) was estimated. If we take an example of Bulgaria, the cost differentials with Estonia had the greatest
weight (0.41), followed by France (0.25), the Netherlands (0.18) and finally Switzerland (0.16).
Finally, costs were extrapolated from the four anchor countries to the remaining ones using cost ratio differentials estimated in Step 2, together with matrix weights estimated in Step 3. The costs were extrapolated for all disease costs, as well as for death-related and residual costs. The costs for injuries were estimated using similar methodology, but using the following countries as the anchor ones: Hungary, Estonia, Greece, Sweden.
